Antimicrobial stewardship (AMS) is essential to combating antimicrobial resistance (AMR)—a growing global health challenge that makes common infections harder, and sometimes impossible, to treat.
By promoting responsible prescription practices and monitoring antibiotic use, AMS delivers coordinated strategies to optimize the use of antimicrobial medicines, ensuring patients receive the right drug, at the right dose, for the right duration.
A well-trained health workforce is the first line of defense against AMR, mitigating inappropriate and excessive use of antibiotics. AMS takes a systematic approach to educating and supporting health care professionals to follow national guidelines for prescribing through training and monitoring.
Building a foundation for AMS in Zambia
To prompt rational use of antimicrobials by health care professionals, expert clinicians and pharmacists develop national legislative and policy frameworks that establish evidence-based treatment recommendations for common medical conditions. These guidelines are regularly updated to reflect emerging evidence and resistance patterns. Updated guidelines are widely disseminated to ensure that health care workers at all levels of the health system are informed and follow the new protocols.
As the Centre for Infectious Disease Research in Zambia’s technical consortium partner for the Fleming Fund Country Grant Phase II, PATH worked alongside the Zambia National Public Health Institute (ZNPHI) and the Zambia Ministry of Health’s pharmacy unit to strengthen national capacity and systems for AMS and antimicrobial use surveillance.
Through this grant, PATH supported the second and third consolidation workshops for the Standard Treatment Guidelines (STGs), Zambia National Formulary, and Essential Medicines List—key policy documents that guide the rational use of medicines across the health system. Once the documents were finalized, PATH supported their dissemination to health care workers throughout Zambia.
Health care workers in Zambia are now equipped with several evidence-based resources to reduce the spread of AMR and enhance patient care and safety. Over time, these updated clinical guidelines will lower health care costs nationwide by curbing the misuse of antibiotics and reducing the burden of drug-resistant infections on the health system.
Furthering awareness through health care worker training
Updating national policies is insufficient on its own to promote AMS. These policies need to be translated into training for physicians, pharmacists, and nurses on how to apply AMS principles to optimize antimicrobial use and prevent infections in their daily practice.
In Zambia, PATH worked with the Antimicrobial Resistance Coordinating Committee—the arm of the ZNPHI responsible for leading the country’s fight against AMR—to deliver an AMS training-of-trainers workshop.
“The training gave participants hands-on tools to monitor prescribing patterns and improve antibiotic use by their patients and the skills to teach others how to use the same tools,” said Benjamin Solochi, PATH Surveillance and AMR Specialist in Zambia.
After the workshop, participants conducted similar trainings at their own hospitals and facilities, providing individualized support to clinicians on safe prescribing practices.
This workshop brought together health care workers from both the private and public sector in Zambia. While much of the focus has traditionally been on the public sector, private hospitals and laboratories also play a vital role in combating AMR.
Health care workers from the private sector learned alongside their colleagues working in the public sector, sharing experiences and best practices on implementing strong AMS programs.
“The collaboration between public and private partners shows that combating antimicrobial resistance requires a united front across the entire health system,” said Dr. Joseph Chizimu, ZNPHI Antimicrobial Resistance National Focal Point and Coordinator in Zambia.
Private health care facilities are joining the fight against AMR. After an initial facility assessment, ten facilities voluntarily joined Zambia’s national AMS program, which will enhance public-private collaboration and ultimately reduce the prevalence of drug-resistant infections and hospitalizations across both systems.
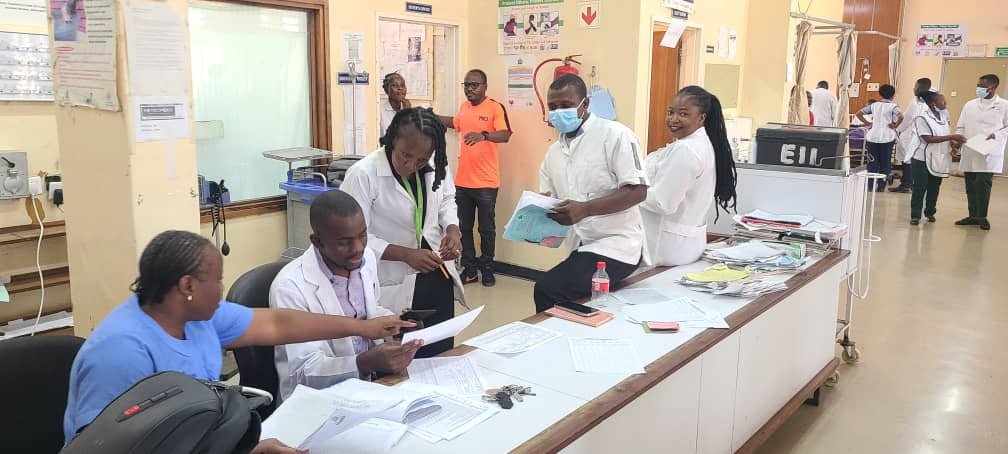
Monitoring prescribing practices at local hospitals
Prescription monitoring within health care facilities is one of the practices of good AMS. Regularly assessing whether medicines are prescribed in line with STGs not only promotes responsible antimicrobial use, but also provides valuable data to shape targeted interventions, influence prescriber behavior, and address emerging prescribing trends.
To advance monitoring, PATH collaborated with national partners in Zambia to conduct a comprehensive prescription audit—a key activity designed to strengthen rational drug use and ensure adherence to updated STGs.
Spanning eight hospitals across eight provinces, the audit reviewed more than 8,000 prescriptions, examining compliance with clinical guidelines, identifying prescribing errors, and analyzing instances of overprescribing and inappropriate antibiotic use.
“The prescription audit gives us a real picture of how antibiotics are being prescribed in hospitals,” said Dr. Chizimu. “It helps us identify gaps, standardize practices, and guide hospitals toward safer, evidence-based care.”
By supporting initiatives like this, PATH and our partners are helping to institutionalize safer prescribing practices in hospitals across Zambia—an essential step toward safeguarding the long-term effectiveness of lifesaving medicines and reinforcing the country’s national AMR response.
PATH takes a multi-pronged approach to AMS that supports the dissemination of clinical guidelines, training of health care workers, and regular monitoring of prescribing practices. Ensuring that safer prescribing practices are driven by a well-informed and coordinated health care workforce, PATH is contributing to slowing down the emergence of drug-resistant infections and ultimately improving patient health outcomes.