In 2021, India’s National Health Authority launched the Ayushman Bharat Digital Mission (ABDM)—a plan to develop an integrated digital health infrastructure and transform the Indian health care landscape for its 1.3 billion citizens.
Based on PATH’s extensive experience of implementing digital health infrastructure in many countries, our team knew that a successful digital health ecosystem can only be created through active participation of both the private and public health sectors.
Driving the adoption of digital health
In 2022, PATH began working with the National Health Authority to onboard private-sector doctors, clinics, and small hospitals on ABDM in Mumbai, Maharashtra. Onboarding consists of registering doctors and clinics/hospitals on ABDM’s Healthcare Professionals Registry and Health Facility Registry, respectively, and deploying the ABDM-enabled hospital management information system (colloquially, an HMIS) for generating electronic health records that are linked to patients’ Ayushman Bharat Health Account (ABHA), which is a unique health account number for Indian citizens.
The ongoing pilot envisions developing a best-practice model for ABDM private-sector engagement that can be scaled up across India. The pilot focuses on onboarding doctors from small clinics who practice modern as well as traditional medicine and might otherwise remain disconnected in the health care ecosystem.
PATH’s previous work with the private sector in Mumbai also reiterated the need for a multipronged approach to engagement. Before the pilot began, we ensured the relevant stakeholders were involved, with clear roles and responsibilities and a true sense of ownership.
These stakeholders included:
- Health technology providers responsible for developing ABDM-enabled clinical HMIS.
- Municipal Corporation of Greater Mumbai, Maharashtra State Office of ABDM, and ward offices.
- On-site team contracted by PATH responsible for active engagement with doctors and their onboarding on ABDM.
- Agency which supported creation of targeted and relevant content for the pilot and ABDM overall.
In health care facilities, on-site project team members visit doctors, sensitize them about ABDM through flipcharts and other outreach material, onboard them on ABDM, and install an ABDM-enabled HMIS for generating ABHA-linked records. Additionally, support staff conduct follow-up visits, assist the doctors and staff with using the HMIS, and ensure that electronic health records are being generated regularly.
Learning with an active feedback loop
Maintaining an active feedback loop was an essential component in the design of this pilot, and it has already resulted in early learnings, described below.
Pilot within a pilot. Unlike larger hospitals, small clinics in the region often don’t use digital clinic management software and tools. For many clinics in this pilot, digital health technologies, such an HMIS, are new and unfamiliar. The pilot would be key in improving usability of the ABDM-compliant HMIS through real-world feedback.
Cognizant of this, we included in the pilot an initial 15-day sprint to ensure that every step was tested at the clinics, giving the team the ability to see what worked and what didn’t. As a result, we were able to identify relevant knowledge gaps and areas of capacity-building, resolve technical challenges, and address the doctors’ areas of concern. This initial sprint helped not only resolve initial hurdles but also to install mechanisms that would help overcome potential hurdles during implementation.
Behavior change of private providers is at the heart of digitization. Why should I join?Is it mandatory to join? Is this a new government dashboard? Our on-site team members often received questions like these. When the pilot was rolled out, there were no tangible incentives for doctors to register. Additionally, few doctors knew about the program, and there was limited access to communication and awareness material at the national level.
To address these challenges, PATH and partners engaged with the doctors to increase awareness of the benefits of digitization and participation in ABDM. PATH regularly organizes sensitization sessions at the ward level by leveraging a network of ward-level staff and engaging doctors’ societies by participating in their events to raise awareness and expedite registration. A push for adoption from local government and professional societies instills a sense of confidence among target private practitioners.
We also identified ABDM champions—doctors celebrated as front-runners for a national-level digital health initiative, who digitized their practices by regularly generating ABHA-linked electronic health records. They were recognized with a certificate from the National Health Authority and were exemplified as role models in our outreach activities.
Operational learnings. As a novel digital health pilot, the team quickly identified and improved operational inefficiencies for a smoother rollout. For example, at first, on-site project managers were reporting day-to-day progress through Google forms. This resulted in poor data quality, making it difficult to ascertain outputs and assess productivity.
To address these challenges, the team designed and developed an internal dashboard to monitor the progress of the pilot more effectively. The dashboard allows users to easily view progress and analyze trends over time. Validation checks during data entry have reduced the chance of human error and improved data quality.
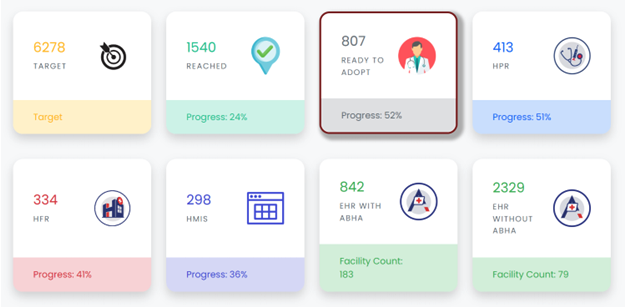
Real-time progress reported via a PATH internal dashboard.
Over the last three months, this project has demonstrated that implementing a digital health initiative requires user-centered solutions, seamless user experience, and effective stakeholder management.
Regular feedback sessions with on-site project managers allowed them to share their experiences, provide insights, and explain practical challenges they faced. Based on their inputs, the pilot facilitated innovations that provided a seamless flow of registration on multiple ABDM modules through a single app. This accelerated the adoption rate and reduced the time that team members spent with each doctor.
Regular trainings updated on-site managers about the latest technology and programmatic developments and encouraged them to think outside the box to improve productivity.
The way forward
The pilot will continue raising awareness about ABDM and engaging doctors to improve the conversion rate and ensure adequate follow-up with already onboarded doctors. This will help establish a self-sustaining ecosystem wherein ABHA-linked electronic health records are continuously generated.
Moving forward, it will be essential to continue evolving the engagement model to ensure maximum private-sector participation in ABDM. The National Health Authority has introduced a new Digital Health Incentive Scheme, which adds financial incentives for more doctors and clinics to join.
In addition, PATH will explore expanding the scope of the pilot to include labs and pharmacies to establish a holistic digital health ecosystem. Citizens will also be actively sensitized about the benefits of digital health records to ensure use of longitudinal health records.



