We are on the cusp of achieving what, for decades, was considered to be unlikely: an effective vaccine against a human parasite. The parasite in question—malaria—has stayed several steps ahead of the human immune system for millennia. While we’ve made great progress shrinking the global malaria map, no single tool will rid the planet of this pernicious parasite, which is why PATH is working on multiple approaches and solutions, including vaccines.
Now, a potentially first malaria vaccine is moving much closer to joining the battle. The World Health Organization (WHO) gave the green light to pilot implementations of the malaria vaccine RTS,S. The WHO-coordinated Malaria Vaccine Implementation Programme will take place in parts of three African countries – Ghana, Kenya, and Malawi -- starting later this year.
Breaking the malaria sound barrier
The development of RTS,S has taken more than 30 years and required overcoming innumerable hurdles that at times seemed insurmountable. Similar to breaking the sound barrier, some said it was impossible to do. But we now know that developing a malaria vaccine is biologically and technically possible.
RTS,S has the potential to prevent millions of cases of malaria, improving the chances of African children to grow up healthy and achieve their full potential, to attend school rather than lie listlessly on hospital cots. RTS,S also represents a scientific breakthrough that can pave the way to the next generation of even more effective vaccines—vaccines that could help make malaria a concern of historians rather than health care workers.
“The next hurdle—pilot implementations of RTS,S—will require significant financing that has yet to be identified.”
What made malaria vaccines so very hard?
First, tough biology. The parasite has more than 5,000 genes, a complex lifecycle, and a sophisticated way of storing its genetic information that’s more like a human’s genome than that of a virus or a bacteria.
It may be a microscopic unicellular organism, but this parasite is a master of adaptability and disguise. To visualize its wiliness, imagine the parasite carries a closet full of clothes to wear. Just when scientists think they’ve found a hole in the parasite’s protective coat, the parasite changes its shirt, tie, and jacket and happily goes its merry way.
Even with repeated infections, humans only develop partial immunity. A child can suffer severe headaches and shaking fevers five or six times in a single year.
The early malaria vaccine heroes
The first milestone on the long road to RTS,S was reached by Ruth and Victor Nussenzweig, a pair of scientists at New York University. In the mid-1980s, after years of research, the duo used early molecular biological techniques to discover a key protein on the surface coat of the malaria parasite—providing a pathway for development of a vaccine.
Fast forward through nearly a decade of research trial (and error) by literally an army of scientists before the next major milestone was reached: six scientists at Walter Reed Army Institute of Research (WRAIR) were vaccinated with an early version of what was to eventually become RTS,S. The results: five out of the six required drug treatment when they fell ill after they were “challenged” with parasite-infected mosquitoes. It was the one subject who didn’t become infected that provided a glimmer of hope.
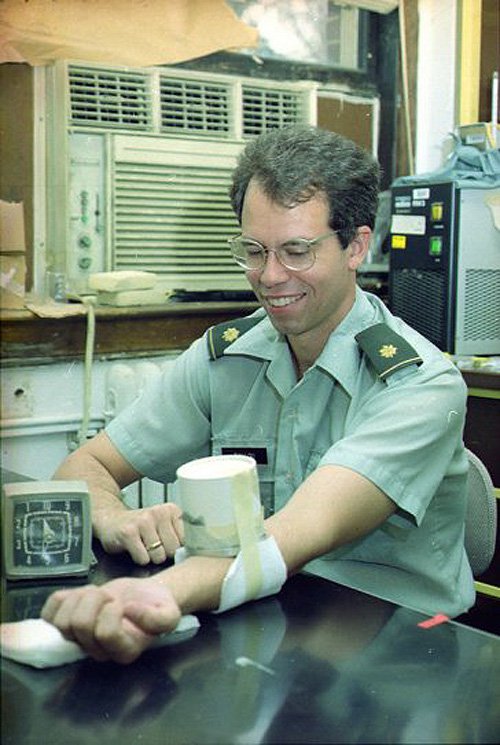
Malaria hero Dr. Ripley Ballou was one of six WRAIR scientists that extended their arms to mosquitoes to test an early version of the vaccine candidate RTS,S. The vaccine prevented malaria for one, not Dr. Ballou. Photo: WRAIR.
RTS,S’s early research was undertaken by GlaxoSmithKline (GSK) in collaboration with WRAIR. Research scientist Joe Cohen and his team figured out a way to boost the immune response and achieve higher protection rates by making a particle with a hepatitis B vaccine and adding a powerful adjuvant. This time, six out of a set of seven subjects administered RTS,S were protected. Hopes rose higher.
A huge hurdle: developing products for a broken market

The malaria parasite may be a microscopic unicellular organism, but with 5,000 genes and a complex lifecycle, it’s a master of adaptability and disguise. Photo: PATH/Will Boase.
One of the largest hurdles to a malaria vaccine is economic. Developing and testing a vaccine can cost US$1 billion or more. Yet a vaccine that will be used against a disease that primarily hits the poorest people in the poorest countries holds out little, if any, opportunity for a financial return, making it a huge challenge for commercial vaccine manufacturers.
In 1999, PATH established the Malaria Vaccine Initiative (MVI) to address market challenges, to share the risk and cost of developing malaria vaccines with partners, and to accelerate malaria vaccine development. RTS,S entered MVI’s portfolio two years later.
MVI created an innovative product development partnership to advance RTS,S, bringing together GSK and scientists from Africa, Europe, and North America. Together, the partners designed an approach that leveraged each party’s strengths from clinical development to research capacity-building to in-country expertise.
Another huge hurdle: proving malaria vaccines work
To really prove that a malaria vaccine is safe and effective, it needs to be tested in large-scale field studies in populations affected by the disease. Called Phase 3 clinical trials, these studies are typically one of the final steps before regulatory review and approval.
There were some who questioned whether African research centers were equipped and ready to perform large-scale Phase 3 trials to current international clinical, ethical, and safety standards. Some doubted that a trial in thousands of infants and children as complex as the one developed for RTS,S—with 11 sites in 7 countries*—could succeed.
But succeed it did. The partners worked together to upgrade clinics and research facilities, install radiology equipment, and improve communications; they held training programs with clinicians on protocols and procedures; and in addition to recruiting study participants, they recruited hundreds of scientists, clinicians, and health professionals who were committed to the cause.
These efforts strengthened the medical and research capacity in African research centers. Perhaps more importantly, they built trust between a network of centers and created a tightly knit community of vaccine researchers across Africa.
When Sam’s son died of malaria, he made it his mission to educate communities in Kenya about the disease. Meet Sam and some of the African scientists, researchers, and community health workers helping advance malaria vaccines in the video.
The youngest malaria heroes
African families strongly committed to the trial as well. More than 15,000 infants and young children were vaccinated. These tiny malaria heroes and their families were as critical to the success of the effort to evaluate the safety and efficacy of RTS,S as were the legions of heroes in the clinics, the labs, and the factory floor who worked tirelessly to administer, test, and manufacture RTS,S.
The trial had a tremendous impact on the communities involved beyond studying RTS,S. One way was through the general health care provided. At one research center, the greater access to health services and quality care, not only for malaria but for a host of illnesses, reduced all-cause mortality in infants and children by an estimated 70 percent!

This child and others enrolled in the RTS,S trial were given mosquito nets, and they and their communities received free health care. Photo: John-Michael Maas/Darby Communications.
Modest protection but significant public health impact
The Phase 3 trial showed that RTS,S was effective at preventing a first or only clinical episode of malaria in 56 percent of young children in the 12 months following vaccination. The protection afforded by RTS,S reduced over time after the first three doses and, for this reason, a fourth dose is recommended.
Given the estimated 200 million people affected by malaria each year—some several times—even a vaccine with limited efficacy, when used correctly alongside insecticide-treated bednets and other interventions, has the potential to prevent millions of cases of malaria and to make a substantial contribution to malaria control, particularly in the settings with the highest malaria burden.
The future of malaria vaccines
As a first-generation vaccine, RTS,S continues to teach us a lot about malaria and vaccines. And 30 years after the Nussenzweigs’ first breakthrough, the malaria vaccine development field continues to be an increasingly vibrant area of scientific learning.
PATH, along with partners around the world, is already working on a next generation of vaccines that could contribute to eliminating malaria. Preliminary results from studies that are evaluating how to enhance the efficacy of RTS,S through changes to dose and schedule look promising, though outcomes from field studies won’t be known for a number of years.
We’ve learned that developing the next malaria vaccine is no longer a question of “if,” but “how” and “when.”

“I would like all children to be able to get the vaccine,” says Mary Okeyo, whose son was enrolled in the study at the Kombewa research facility in Kenya. Photo: PATH/Teresa Guillien.
Next hurdle: “if” and “when” to impact
Which raises the next hurdle that RTS,S faces. Despite a positive scientific opinion from the stringent European regulatory agency and despite WHO’s recommendation for pilot implementations of RTS,S, the broken market still exists—pilot implementations of RTS,S will require significant financing that has yet to be fully identified. Generous contributions from Gavi, the Vaccine Alliance; the Global Fund to Fight AIDS, Tuberculosis, and Malaria; and UNITAID, will get us through the first phase of pilot implementation. Hopefully there will soon be answers to “if” and “when” support will be available so we can reach the next milestone on the road to the first malaria vaccine: impact.
In the meantime, we at PATH thank the many malaria heroes who have driven RTS,S this close.
* Burkina Faso, Gabon, Ghana, Kenya, Malawi, Mozambique, and Tanzania.



