Integrated disease surveillance systems form the foundation of global health security. They enable early detection of outbreaks, prevent epidemics from escalating into pandemics, and support evidence-based responses. Yet in practice, many systems falter due to fragmentation across diseases, departments, and funding streams.
Siloed programs targeting tuberculosis, polio, neglected tropical diseases (NTDs), malaria, measles–rubella, HIV, and diarrheal diseases, while effective in achieving disease-specific goals are resource-intensive over time. They often result in duplication of efforts within the same communities, drawing on a shared health workforce and infrastructure, and placing avoidable strain on health systems. Such fragmentation limits efficiency where integrated and combined surveillance could offer greater value.
As donor funding contracts and the threat of emerging and re-emerging infectious diseases intensify globally, countries must shift toward integrated disease surveillance mechanisms. These systems are essential to strengthen preparedness, enable effective case management, and ensure timely responses that prevent outbreaks from spreading addressing multi-etiologic communicable diseases through a coordinated, convergent approach within a single health system serving the same populations.
Accelerating progress across South Asia
Robust systems generate key epidemiologic parameters with time, place, and person-specific data, giving insights into which pathogens are circulating and how quickly response measures must be deployed. Across South Asia, gaps in disease surveillance, ranging from fragmented data systems to limited laboratory capacity and uneven distribution of human resources, have hampered efficient response. Yet the region is increasingly demonstrating how these challenges can be addressed through more integrated, multi-sectoral approaches to disease surveillance.
Bangladesh has strengthened surveillance for influenza, Nipah virus, antimicrobial resistance, dengue, and acute febrile illness, supported by field epidemiology training and laboratory facilities. PATH, in collaboration with the Ministry of Health and the World Health Organization (WHO), developed and piloted a post-validation surveillance (PVS) toolkit for lymphatic filariasis. This uses existing systems to monitor NTDs post-elimination, converging data to expand integrated surveillance across other NTDs as well.
Additionally, PATH supported Nepal’s COVID-19 response through environmental surveillance of sewage to detect and monitor the spread of COVID-19.
Uttar Pradesh: Integration at scale
India is advancing large-scale integration through the Integrated Disease Surveillance Programme (IDSP) and countrywide digital platforms, such as the Integrated Health Information Platform (IHIP). IDSP is a flagship initiative of the National Health Mission to strengthen decentralized, IT-enabled, laboratory-based surveillance to track epidemic-prone diseases and enable early outbreak detection and response.
In the state of Uttar Pradesh (UP), there is a significant burden of infectious diseases, including AES, which disproportionately affects children with rapid progression to death or disability for variable etiologies. Case fatality rates exceeded 20% due to low awareness, delayed care-seeking, weak primary health care response, and fragmented surveillance systems having sub-optimal monitoring-feedback and supportive supervision.
To address this, UP launched a Unified Disease Surveillance Platform, which links labs, facilities, and communities under the IDSP. Its High-Grade Fever Surveillance Model integrates testing for six etiologies of Chikungunya, Dengue, Japanese Encephalitis, Leptospirosis, Malaria, and Scrub Typhus for each suspected AES case.
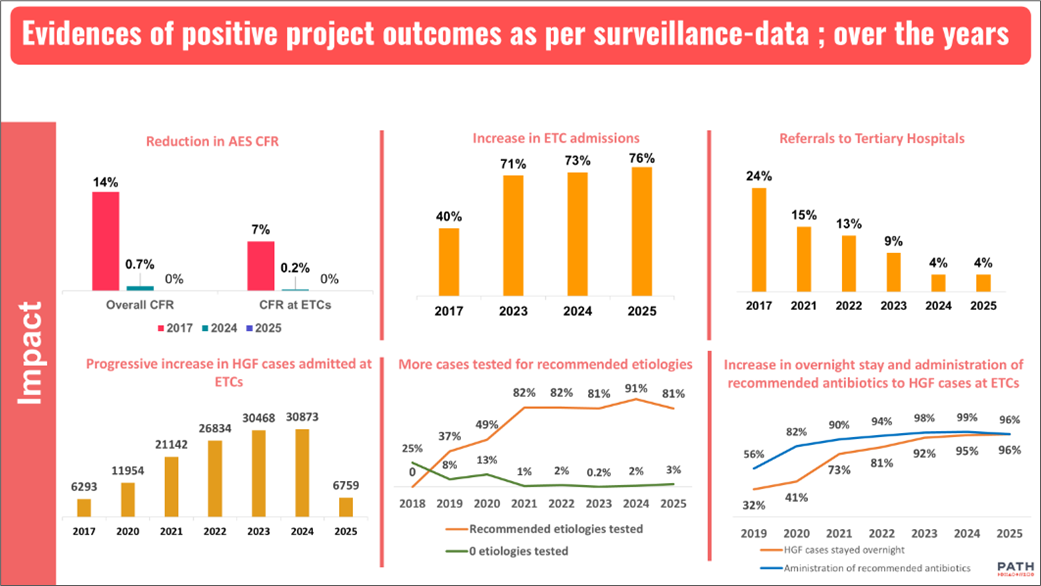
With support of the Gates Foundation, PATH with partners like WHO and UNICEF provided technical assistance to establish and strengthen Encephalitis Treatment Centers in 18 high-burden districts of the state. This included equipping primary health care facilities with basic essential diagnostic devices, medicines, oxygen, and well-trained health staff to reduce reliance on tertiary hospitals.
The state-implemented community drives are also amplifying impact. The DASTAK program sends field workers to every household three times yearly for fever screening and sensitization. It integrates with Sanchari Rog Niyantran Abhiyan (SRNA), converging 14 government departments quarterly to prevent outbreaks in villages and urban wards. This convergence of data, diagnostics, and delivery enables earlier detection, faster referrals, and effective control, most evident in the AES response.
Results have been promising.
AES cases declined from 4,724 in 2017 to 81 by May 2025; deaths fell from 655 to zero (January–May 2025). Case fatality dropped from 14% to <1%. ETCs reduced tertiary referrals by over 80% and minimized treatment delays.
PATH supported master trainer pools, updated modules, and standard operating procedures. Surveillance saves lives when integrated with laboratories, frontline health care providers, communities, and leadership, turning data into timely decisive action.
Lessons for global health security
Uttar Pradesh’s AES model offers scalable insights:
- Strengthen existing systems: Build on primary health centers, district labs, and well-trained and well-equipped frontline health workers.
- Mandate multi-etiology testing: Prepare for known and emerging threats through an integrated laboratory network testing for a multi-etiological fever surveillance system
- Ensure inter-departmental coordination: Align health departments, labs, medical colleges, and non-health sectors like veterinary, agriculture, urban development, rural development, water-sanitation, and others through clear governance and accountability.
- Protect broader populations: Integrated systems safeguard against both communicable and noncommunicable diseases with comorbidities during outbreaks, as COVID-19 highlighted.
With declining donor funds, climate-driven risks, and antimicrobial resistance, integrated disease surveillance, grounded in local action, is a high-impact investment and the way forward in the future.



