2025 was a year that asked a lot of all of us in global health. Funding landscapes shifted beneath our feet, long-standing challenges like climate change and antimicrobial resistance grew more urgent, and the systems we rely on were pushed harder than ever.
What could have been a year defined by constraint instead revealed something deeper: our collective resilience, our creativity, and our commitment to showing up for communities no matter the circumstance.
Across the sector, and across PATH, people met uncertainty with collaboration. Partners stepped in. Teams stretched, adapted, and found new ways to solve problems. And as health budgets tightened, the value of relationships, trust, and shared purpose became even more evident. We were reminded that innovation isn’t only about technology or tools—it’s also about the courage to reimagine what’s possible when resources are scarce and needs are great.
PATH entered this year with a clear mission: to deliver life-saving solutions and expand access to quality health care, especially for those too often left out of traditional systems. What emerged over the months was a body of work that reflects not only technical strength but a deep sense of humanity—meeting people where they are, listening closely, and designing with intention.
Here are a few of the moments and achievements from across PATH in 2025 that remind us what resilience looks like in practice.
Realizing the power of strong partnership

PATH staff, Rotarians, Rotary Foundation staff, community health workers, and health facility staff during an RHCC site visit in Akwa Ibom, Nigeria. Photo: PATH.
In Nigeria, partnership came to life. Together with community health workers, state leaders, Rotary International, and the Gates Foundation, PATH helped expand integrated child health services across Akwa Ibom and Kebbi states. Through the Rotary Healthy Communities Challenge, Rotary brings the reach and spirit of a global and local movement, the Gates Foundation fuels catalytic investment, and PATH delivers the science, systems, and local expertise to strengthen services in clinics and communities.
As a result, community health workers are supporting families, parents are recognizing danger signs earlier, and data systems are making every child visible—all in service of giving every child the chance to grow and thrive.
Designing integration that meets people where they are
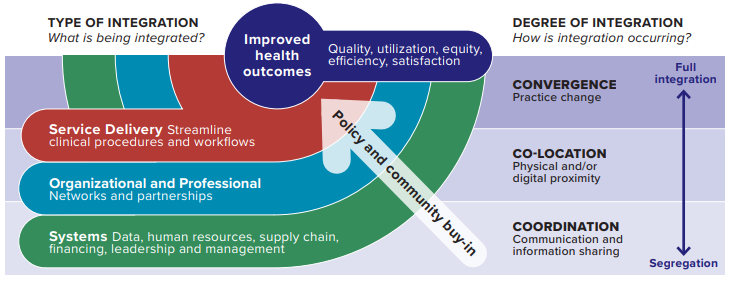
Conceptual framework. Framework adapted from Valentijn et al., 2013 Rainbow Model for Integrated Care; Grépin and Reich, 2008, Degree of Integration; and Heath et al., 2013, Levels of Collaboration.
Integration in health care can mean many things, but at its core it is about shaping systems to deliver care to people where and when they need it.
For years the idea has outpaced the guidance, so PATH created the Integration Primer—a practical framework to help governments and partners understand what to integrate and how to do it well.
This year, that understanding came to life in Indonesia, where PATH worked with national and local leaders, health providers, and communities to co-design an enhanced training approach for community health workers. Together, we built an integrated, life course model supported by a digital decision tool that mirrors real household visits.
The result is training that better matches community health worker needs, digital prompts that support timely referrals, and strengthened skills to deliver holistic care. More families are now reached with essential screening, follow up, and health education, and communities are seeing meaningful improvements in health and confidence in care.
Building sustainable diagnostics in Africa

Robert Matiru (Unitaid), Faith Mangwanya (Unitaid), Perrer Tosso (USP), Boitumelo Semete-Makokotlela (SAHPRA), Jamil Barton (PATH), and Jens Pedersen (AfCDC) discuss the MADE Project at the African Healthcare Manufacturing Trade Exhibition and Conference.
In 2025, Africa took a powerful step toward self-reliance in health technology. With support from Unitaid and partners across the continent, PATH launched the Manufacturing to Accelerate Diagnostic Excellence (MADE) project—a collective effort to build a durable diagnostic manufacturing base and reduce dependence on imported products.
Working alongside the African Society for Laboratory Medicine, Solina Centre for International Development and Research, the University of Cape Town, WACI Health, and Open Capital, we are helping African companies design, produce, and scale up high-quality diagnostic tests for regional and global markets.
By strengthening access to raw materials and enabling manufacturers to control more of their supply chains, MADE is laying the groundwork for a future where lifesaving diagnostics are created closer to the communities they serve—and where African innovation anchors global health resilience.
A safe beginning for every child

Women attend a discussion about nutrition and breastfeeding at a hospital. Photo: PATH/Evelyn Hockstein.
We took an important step toward a future where no child is born with a preventable disease. With support from Unitaid, PATH launched SAFEStart+—a $25 million effort to integrate screening and treatment for HIV, hepatitis B, syphilis, and Chagas disease into routine antenatal care.
Working with community leaders and delivering care in the places where women already seek support, SAFEStart+ strengthens the systems that protect mothers and babies. In partnership with the World Hepatitis Alliance and the International Community of Women Living with HIV Eastern Africa, and with technical leadership from the World Health Organization (WHO) and the Pan American Health Organization (PAHO), the initiative will advance people-centered solutions across nine countries (Brazil, Democratic Republic of the Congo, Malawi, Nigeria, Paraguay, Senegal, South Africa, Uganda, and Vietnam), helping ensure every child has the chance to begin life healthy and safe.
The power of self-care

Program Manager Allen Namagembe from PATH’s Uganda office at the Evidence2Practice workshop in Addis Ababa, Ethiopia. Photo: PATH
Scaling up a product is never just about introduction—it is about listening, learning, and anchoring every step in equity.
In 2025 that approach came into sharp focus as PATH and Ethiopia’s Federal Ministry of Health convened the Evidence2Practice workshop, bringing together more than 90 partners from 14 countries to reflect on what it takes to expand access to DMPA-SC, the all-in-one self-injectable contraceptive that puts agency directly into women’s hands.
The evidence is clear: when women can self-inject, they gain time, autonomy, and the freedom to choose what their futures look like. Expanding access to this tool means more women shaping their own paths, as well as health systems evolving to meet them with dignity, care, and possibility.
Anticipating the next crisis
PATH
This year taught us that, now more than ever, it is vital to build smarter, connected systems that can adapt and endure using innovation grounded in trust and designed for the long haul.
The Global Goods Guidebook Annex exemplified this approach, connecting climate intelligence, health data, and open-source tools to help country leaders improve capacity to create predictive models, identify early threats such as extreme weather and heat, and build smarter, faster, targeted responses.
Developed under the PATH-led Digital Public Infrastructure for Climate and Health (DPI4CH) project, the guidebook is part of a broader initiative funded by Wellcome and the Rockefeller Foundation, in collaboration with the World Health Organization (WHO) – World Meteorological Organization (WMO) Climate and Health Joint Programme, to improve knowledge sharing across climate and health experts and identify and share climate-informed trusted digital tools for health.
Celebrating new beginnings

The ribbon-cutting ceremony at the new PATH office in Seattle. Photo: PATH/Dave Simpson.
In 2025, PATH returned to its beginnings. Nearly 50 years after opening our first office along the Lake Washington Ship Canal, we came home—this time to a space built for the future of global health.
Our new Seattle headquarters brings together our Biosafety Level 2 lab for advancing vaccines, diagnostics, and mRNA platforms and our hands-on engineering shop where teams prototype and refine tools for low-resource settings.
From this hub—connected to colleagues and partners in 70+ countries—we move ideas into action, expanding access and strengthening systems for the more than 64 million people we reach each year.
Closing the oxygen gap

PATH staff deliver oxygen supplies from the Oxygen Delivery Gap Fund to Tumbi Regional Referral Hospital in Kibaha, Tanzania, which serves a population of over 2 million. Photo: PATH.
Medical oxygen—one of the most essential yet frequently unavailable tools for saving lives—cannot afford to be overlooked by country governments and global decision-makers in their health agendas, as it underpins effective care across entire health systems. The consequences of oxygen shortages are felt most acutely by patients in respiratory distress, by newborns struggling to breathe, and by mothers experiencing complications during childbirth.
The Oxygen Delivery Gap Fund, a workstream under PATH’s Strengthening Oxygen Utilization and Respiratory Care Ecosystems (SOURCE) project co-funded by the Gates Foundation and the ELMA Foundation, completed the delivery of critical respiratory care equipment to health facilities in the Democratic Republic of the Congo, Kenya, Malawi, Tanzania, and Zambia. To understand how these resources were being used—and what additional support was required—PATH conducted rapid impact assessments across 11 facilities within 30 days of delivery. These assessments examined whether the equipment was reaching the patients who needed it most, whether health workers had adequate training and support, and whether systems were in place to manage and sustain these investments over time.
SOURCE concluded in 2025 after more than four years of implementation across ten geographies. Over the life of the project, 119,101 pieces of equipment were procured, 1,136 facilities were surveyed, and 17,830 health workers were trained.
Reaching the unreached

A community health worker administers antimalarial treatment to treat a case of malaria as part of proactive community case management in Pujehun District, Sierra Leone. Photo: PMI Insights.
The burden of malaria remains profound, touching families and communities across continents. Yet the PATH-led REACH Malaria project (funded by the US Government) continues to hold steady. REACH strengthens the planning, delivery, quality, and monitoring of malaria services in regions of Africa and Asia where the need is greatest, and it helps bring critical care to women and children living hours from the nearest health facility.
This year, REACH expanded from 11 to 22 countries, delivering lifesaving antimalarial treatment to more than three million children under age five through seasonal malaria chemoprevention campaigns in Ghana, Mali, and Togo. The project also trained more than 3,000 health care providers across malaria case management, severe malaria care, integrated community case management, and malaria in pregnancy, while supporting vaccine introductions in Liberia, Mali, Togo, and Zambia through planning, training, community engagement, and post-introduction evaluations that strengthen long-term use.
Together with ministries, communities, and frontline workers, REACH is bringing effective tools closer to home and moving us toward a world where no child’s life is shaped or limited by malaria.
Reimaging care through responsible AI

The clinical decision support tools evaluated as part of PATH-led research trials in Kenya, Rwanda, and Nigeria in 2025. Image: PATH/Jen Fox.
With the Gates Foundation and partners in Kenya, Nigeria, and Rwanda, we launched clinical trials that reimagine how AI can advance health equity. These large language model (LLM) tools aren’t designed to replace providers—they’re built to strengthen them, offering real-time clinical support in settings where resources are stretched and time is scarce.
Early results point to something powerful: technology that meets people where they are, supports the workers who hold health systems together, and brings accurate, dignified care within reach for more communities.
Strengthening the systems that keep us safe

Dr. Laura Lydia Adong (khaki overalls), a veterinary officer in Uganda, vaccinates farm animals against anthrax. PATH helps governments apply a One Health approach to guard against climate-driven zoonotic disease outbreaks. Photo: PATH/BBCStoryWorks.
Emerging diseases do not respect borders, so the systems that protect us cannot afford to either. This year, PATH’s epidemic preparedness and response portfolio grew in powerful ways, expanding support across Africa, Asia, and Latin America.
Through STRIDES (an activity funded by the US Department of State), we are helping the countries we partner with strengthen surveillance, bolster data and laboratory systems, and respond quickly when new threats arise.
And in Cambodia, the launch of the KfW-funded One Health 4 Cambodia initiative marked the beginning of an integrated approach to tackling antimicrobial resistance, zoonotic disease, and emerging infections. Together, these efforts build the foundations of readiness through systems that see earlier, act faster, and keep communities safer.
A global community for the earliest years

Childcare Advocacy, Research, and Engagement (CARE) Initiative partners at a workshop in Bangladesh. Photo: BRAC Institute of Educational Development.
Caring for young children asks all of us to think bigger than any single sector. It means building bridges across movements, sharing what works, and fighting for the policies and resources families deserve. That’s why PATH continues to host the Early Childhood Development Action Network—the only global network devoted entirely to the holistic needs of young children and their caregivers.
This year, ECDAN grew to 381 organizational partners across 66 countries and a community of nearly 50,000 people learning, advocating, and creating together. As funding uncertainty threatens the early years, the network is doubling down—mobilizing domestic and complementary financing, championing systems approaches, integrating early childhood into climate action, and equipping local advocates to lead cross-movement coalitions. This is collective work in service of a simple truth: every child deserves the chance to begin life with safety, connection, and possibility.
Strengthening coordination for a smarter, faster malaria response

Members of the PATH malaria team during a work planning session in Cape Town. Photo: PATH.
The PATH Malaria Control and Elimination Partnership in Africa (MACEPA) helped anchor coordination across the malaria community this year, working with governments and partners to realign resources, sharpen priorities, and keep essential efforts moving forward.
The team advanced new tools that make data work harder for countries, including SnapForm, an AI-driven solution that cuts reporting time, improves accuracy, and reduces costs, and a user-friendly budgeting tool that helps model intervention mixes and visualize tradeoffs.
MACEPA also launched a multi-country data fellowship, building a new generation of analysts who are strengthening malaria programs from the inside out. Together, these efforts are helping countries make faster, clearer decisions and bring effective malaria tools closer to the communities that need them most.
This work is only possible because of the people who carry it forward every day.
To the communities at the heart of everything we do, to the partners and governments that walk alongside us, and to the colleagues across PATH who bring courage, creativity, and care to every challenge—thank you.
Your commitment turns uncertainty into progress and keeps hope moving, even in the hardest years.
As we look ahead, I am grateful for the shared purpose that grounds us and the collective resilience that continues to shape a healthier, more just world.
Here’s to the communities who guide this work, and to all of you who refuse to stop imagining what is possible.