Noncommunicable diseases (NCDs) kill 43 million people each year, which makes up 74 percent of all global deaths. Up to 80 percent of these deaths are preventable with proven interventions, yet less than 2 percent of global financing goes toward these conditions.
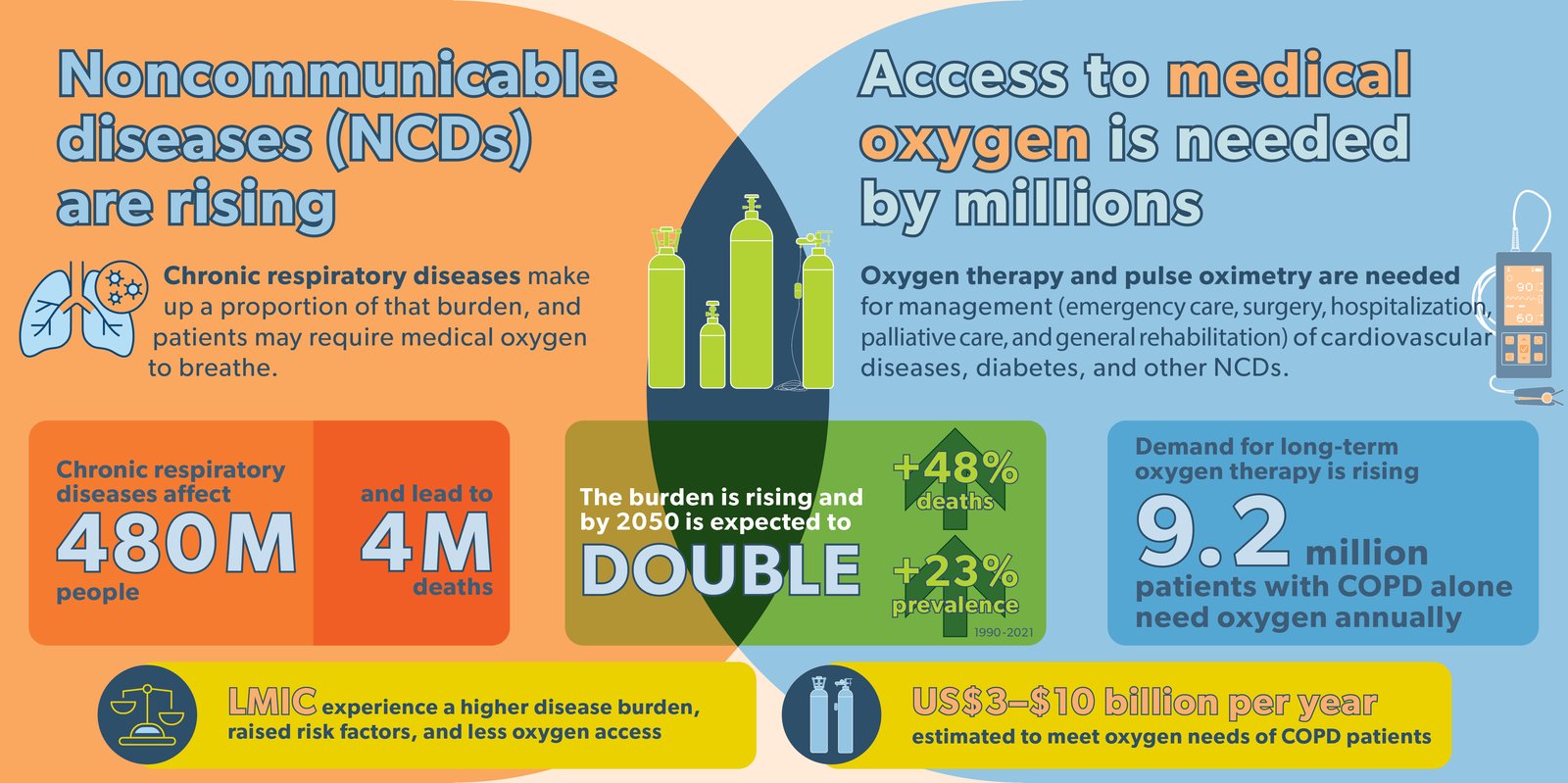
Chronic respiratory diseases—like chronic obstructive pulmonary disease (COPD), interstitial lung disease, and pulmonary hypertension—make up a significant proportion of those deaths each year. Many of these patients require medical oxygen to breathe. Beyond this, oxygen therapy and pulse oximetry are needed for the management of cardiovascular diseases, diabetes, asthma, and other NCDs, as part of emergency care, surgery, hospitalization, imaging, and palliative care, as well as general rehabilitation.
While the World Health Organization recognizes medical oxygen as critical for numerous NCDs, this essential medicine is often missing from conversations, global agendas, and investments to address these health conditions.
Country governments and global decision-makers cannot afford to overlook this missing piece in their NCD agendas. Here’s why:
1. NCD rates are rising, with inequitable burden and access to reliable treatments like oxygen
Each year, the burden of disease and deaths continue to shift from communicable to noncommunicable diseases, especially in low- and middle-income countries (LMICs). For chronic respiratory diseases, total deaths have increased by 48 percent between 1990 and 2021. These conditions affect over 480 million people, including 96 million children under 15 years of age, and are responsible for more than 4 million deaths each year—making them the third highest cause of death globally. This burden is forecasted to double by 2050.
Smoking, followed by air pollution and occupational exposure, contributes to the majority of illness and deaths from chronic respiratory diseases; these risk factors are often elevated in LMICs. Many countries are falling behind in meeting global targets for universal health coverage and access to essential medicines and supplies for NCDs like chronic respiratory diseases, widening health inequities between and within countries. This includes access to oxygen as a treatment in health facilities and at home.
2. Millions of patients need long-term oxygen therapy, and demand is rising
Many patients with chronic respiratory disease require long-term oxygen therapy to breathe, particularly those with COPD. An estimated 9.2 million people with this condition require oxygen annually, with two-thirds living in LMICs. Each of these individuals requires a continuous portable oxygen supply; yet, almost no one who needs long-term oxygen therapy in LMICs receives it due to its overwhelming cost or a lack of a reliable power source, like electricity. In fact, these patients are often admitted to hospitals solely due to their inability to access oxygen at home.
The number of people needing long-term oxygen therapy grew by 33 percent between 2010 and 2021. This demand is expected to continue increasing, with the projected 23 percent rise in COPD between 2020 and 2050, disproportionally impacting those living in LMICs.
The annual cost to meet the long-term oxygen needs for COPD patients alone is estimated at US$3 to $10 billion—a sum that is out of reach for many countries. Without sufficient action, the rising burden and infeasible cost will deepen broader inequities in access to this critical treatment.
3. Oxygen access must be matched with broader prevention and risk reduction measures
The rising burden of chronic respiratory disease is due to long-term effects of smoking on an aging population and exposure to indoor and outdoor air pollution, exacerbated by climate change and urbanization. Given the high cost of long-term oxygen therapy, strengthening oxygen delivery systems must be complemented by preventative measures to curb major risk factors.
Mitigating these risks ranges from tobacco control to improving outdoor air quality, advancing clean cooking and heating fuels, and reducing occupational hazards that can damage respiratory health. Initiatives to lessen transmission of interrelated communicable diseases, like tuberculosis, are also vital.
Access to and use of long-term oxygen therapy means appropriately planning for and then maintaining a mix of oxygen infrastructure to support both facility- and home-based care, building on primary health care platforms to make oxygen more convenient for patients. This requires better access to complete data, consistent guidelines, context-adaptive approaches, and innovative oxygen-delivery and -conserving systems and technologies.
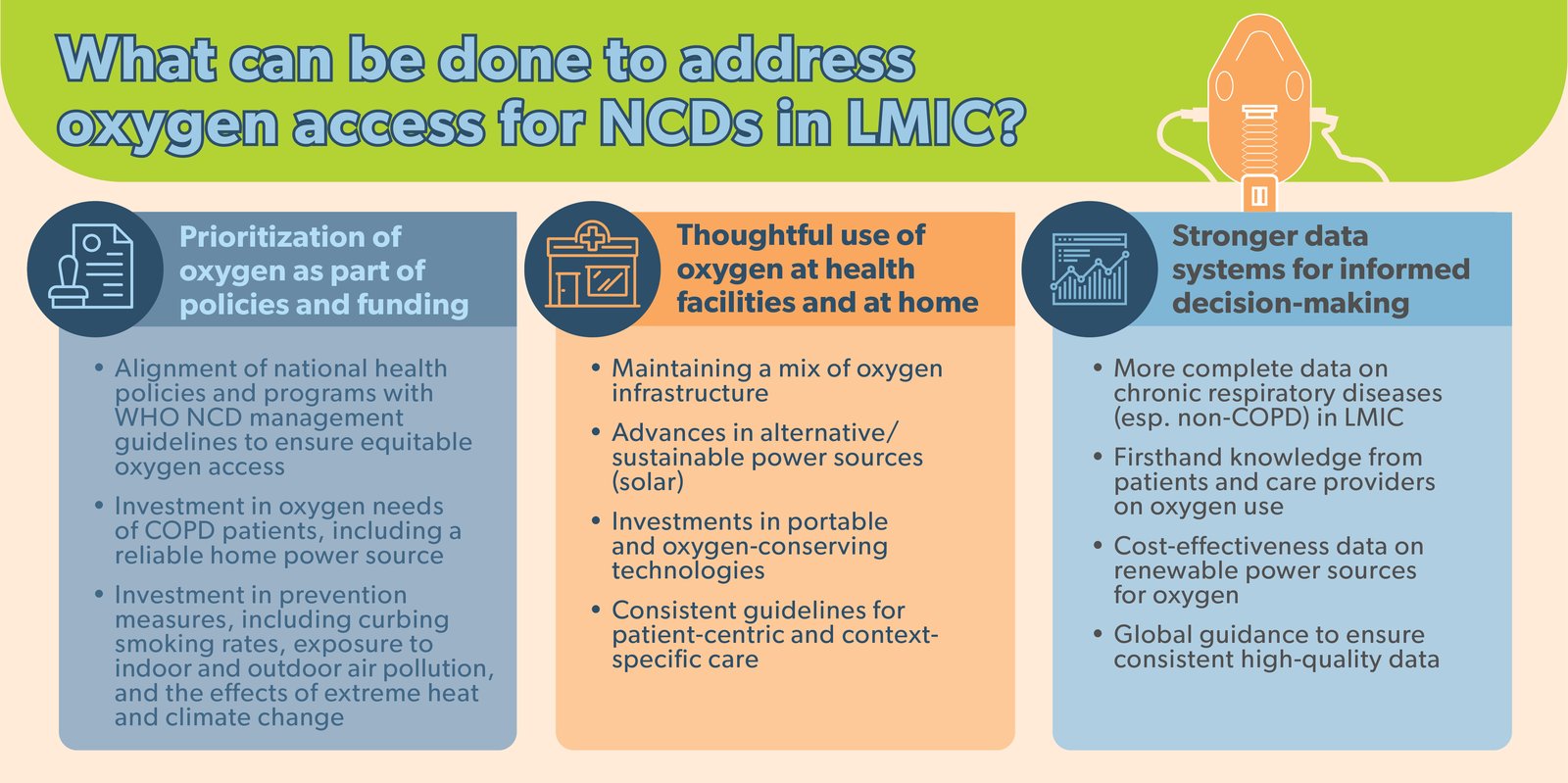
Rising rates of NCDs and corresponding pressure on reliable oxygen ecosystems, limited access to home long-term oxygen therapy, elevated disease risk factors, and inadequate data-driven decision-making all complicate efforts to address the high burden of chronic respiratory diseases in LMICs. More than ever, timely and robust planning for reliable oxygen delivery in health facilities and at home is needed to protect and save lives.
As we work to advance progress for universal health coverage and reduce the burden of NCDs, putting strong medical oxygen systems at the forefront of global health is critical. National governments, donors, advocates, and implementers all have a role to play in supporting LMIC to improve access to high-quality oxygen therapy to ensure every patient receives the appropriate respiratory care at the right time.



