2019 marked an exciting milestone for child health: the rollout of the first malaria vaccine in Ghana, Kenya, and Malawi. This pilot introduction, known as the Malaria Vaccine Implementation Programme, aimed to evaluate the feasibility, safety, and impact of the vaccine in real-life childhood vaccination settings. Coordinated by the World Health Organization (WHO), with technical support from PATH and other partners, the pilot program offered invaluable insights about the impact of malaria vaccines and how to overcome challenges to implementation.
Six years later, the lessons learned during the pilot program are informing the rollout of malaria vaccines in two dozen countries. As of November 2025, 24 countries have introduced the vaccines, with a total of more than 47 million doses delivered so far. PATH is currently working with several countries, including Burkina Faso, Democratic Republic of the Congo (DRC), Mozambique, Nigeria, and Uganda, to provide technical assistance to optimize uptake of the full malaria vaccine schedule.
Unique challenges, tailored solutions
Introducing any new vaccine presents challenges, but malaria vaccine implementation is particularly complex given the vaccination schedule. WHO recommends a schedule of four doses in children from around 5 months of age. However, there can be flexibility in the schedule to optimize delivery: for example, aligning the fourth dose with other vaccines given in the second year of life.
Further, WHO recommends that since no single tool prevents all malaria cases, countries can achieve the greatest impact by providing a mix of malaria interventions, strategically layered and tailored to the local context. In line with this recommendation, malaria vaccines are provided as part of a package of interventions that includes insecticide-treated nets (ITNs), indoor residual spraying, larviciding, and seasonal or perennial malaria chemoprevention.
To address these considerations related to malaria vaccines, PATH helps countries shape strategies that reflect local conditions, policies, and realities—taking into account each specific country context and existing health system structures.
Working locally with communities
Often, developing tailored solutions means working with community members themselves. In the DRC, which introduced the malaria vaccine in October 2024, findings from a knowledge, attitudes, and perceptions (KAP) survey conducted with the Ministry of Health (MOH) showed that only 50 percent of caregivers understood the correct dose schedule for malaria vaccines. Persistent misinformation, lack of trust, and access barriers undermined uptake of the vaccine in the early stages of introduction.
In response, PATH collaborated with the MOH on an approach that involved more than 100 non-traditional partners (NTPs) in Kongo Central, the first province to introduce the vaccine. Working with the country’s Provincial Health Division, PATH led co-creation workshops that brought together representatives from schools, faith groups, local media, women’s and youth associations, and traditional leadership.
During the workshops, these groups brainstormed communication and mobilization strategies aimed at improving malaria vaccine uptake, which included everything from school-based parent engagement to radio broadcasts and community dialogues. NTPs signed commitments to carry out these activities, and PATH and the MOH have continued to engage with them to monitor progress and offer support with training and tools.
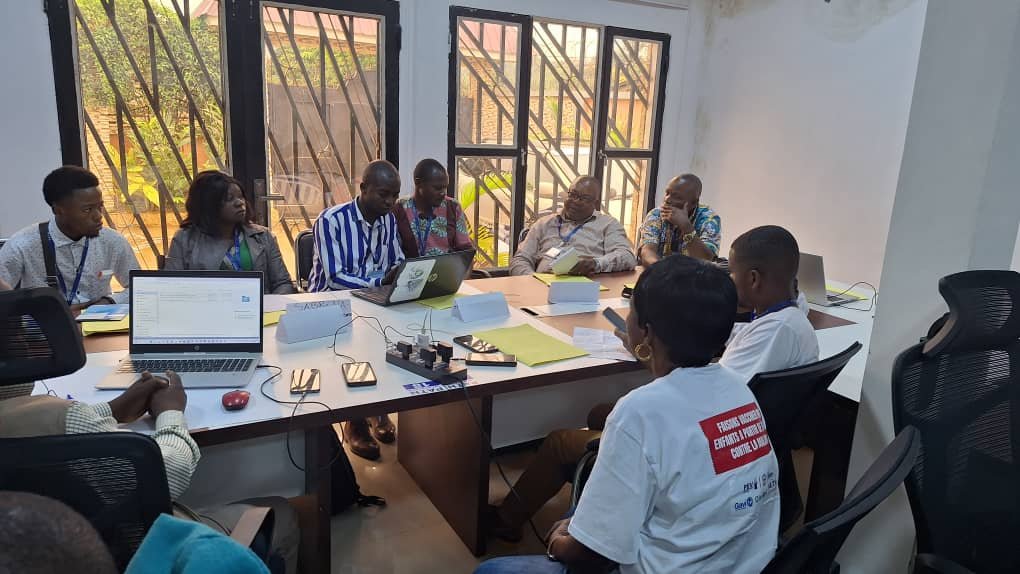
PATH and the DRC Ministry of Health held a co-creation workshop in Mbanza Ndungu, Kongo Central, with non-traditional partners from four health zones of the EPI branch. Credit: PATH.
Leveraging data for decision-making
Improving data capture and use is an essential part of PATH’s technical assistance approach. Accurate data is critical to informing supply decisions, monitoring vaccine uptake, and identifying and supporting areas with low coverage or high dropout rates.
In Mozambique, PATH conducted a data quality assessment in eight districts of Zambezia Province in May 2025. The assessment revealed inconsistent data quality on malaria vaccines across child immunization recording tools, with discrepancies observed in logbooks, tally sheets, monthly summaries, and the DHIS2 software platform.
In response, PATH is training health care providers in Zambezia on data quality improvement and designing health facility action plans to resolve issues. PATH has held data quality trainings for more than 50 participants from six districts in Zambezia and is continuing to provide monthly supervision and mentoring, including in-person, on-the-job training for health care providers. Alongside the data quality trainings, PATH staffers have also used site visits as an opportunity to implement malaria vaccine communication and demand generation strategies within communities.

A data quality improvement training in Pebane District, Zambezia Province, Mozambique. Photo Credit: PATH.
Learning from experience
Introducing the four-dose malaria vaccine into an already crowded immunization schedule poses challenges, but identifying roadblocks along the way allows PATH and its partners to course-correct and apply lessons learned. As more countries scale up implementation of malaria vaccines, these learnings are shaping smarter, more responsive strategies.
PATH works in collaboration with WHO, UNICEF, and other partners to develop tools and resources for malaria vaccine rollout. WHO’s Essential Training Packages for Malaria Vaccine Introduction covers key topics for health workers in PowerPoint documents that can be downloaded and customized to meet specific country needs. In addition, TechNet-21 houses a curated summary of technical resources on the current global recommendations, evidence, and programmatic considerations for malaria vaccine introduction into national immunization programs.
By applying insights from early implementation, tailoring approaches to local contexts, and strengthening data systems, PATH and its partners are helping ensure that malaria vaccines reach the children who need them most—saving lives and building more resilient health systems across Africa.



