In the Democratic Republic of Congo (DRC), routine immunization efforts face a hidden but significant barrier: fear and mismanagement of adverse events following immunization (AEFIs). For many parents, a child’s fever after vaccination is not just a health concern, it’s a financial burden. These concerns result in some caregivers opting out of vaccination altogether, contributing to the persistence of zero-dose children (children who have yet to receive a dose of vaccine).
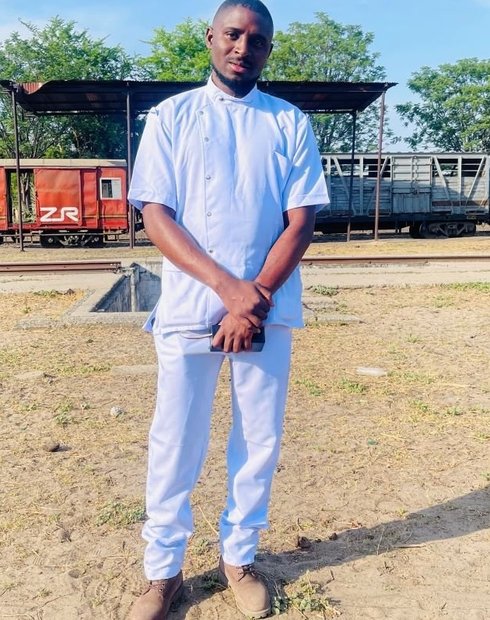
In the Kabondo Health Zone, PATH’s Living Labs team, in partnership with local stakeholders, used a human-centered design (HCD) approach to co-create solutions to this challenge. Chief Medical Officer Dr. Dhoho Shuku Herman became a key champion, guiding the process and ensuring the solutions reflected community needs and realities.
Issues undermining vaccination coverage
Before this intervention, three main issues undermined vaccination coverage in the region:
- No free care for children who developed a fever or other minor side effects post-vaccination.
- Lack of follow-up after vaccination to check on children’s well-being.
- Absence of nearby care facilities equipped to manage AEFIs, especially in rural areas.
These gaps fueled parental hesitation, especially among those already reluctant to vaccinate.
“Before using HCD, we were subject to prescribed activities to solve the problem, unlike HCD, which engages stakeholders in co-creating local solutions to local problems.”— Dr. Dhoho Shuku Herman, Chief Medical Officer
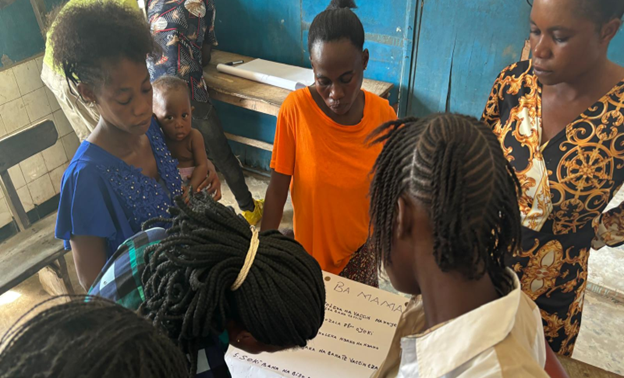
Caregivers providing their perspective and expectations at the co-creation workshop in BCZ Isangi (Central Office of the Isangi Health Zone). Photo: PATH/Living Labs.
Shaping safer vaccination through community voices
The Living Labs team applied the HCD process from start to finish, ensuring that the voices of caregivers, health workers, and community leaders shaped every stage.
Key milestones included:
- Gathering insights through focus groups and interviews with caregivers of zero-dose children, service providers, community relays, religious leaders, and local authorities.
- Conducting a co-creation workshop using proven design tools like Rose-Bud-Thorn analysis, the Five Whys technique to uncover root causes, and Crazy Eights to brainstorm potential solutions.
- Prototyping solutions and testing them with users, iterating based on feedback until high-fidelity concepts emerged.
This approach allows the team to better understand the real problems in vaccination and make good decisions with all actors involved.
Through co-creation, stakeholders identified and prioritized a single integrated intervention for AEFI prevention and management. This included:
- Administering paracetamol after vaccination and providing doses for home use.
- Listing vaccinated children for follow-up.
- Conducting home visits by community health workers to monitor children post-vaccination.
- Ensuring free treatment for any AEFI cases.
These measures addressed both the medical and trust barriers that previously deterred parents from bringing their children for vaccination.
“Half of our population seeks care in private facilities, so integrating them into vaccination recovery for zero-dose and under-vaccinated children was essential.”— Dr. Dhoho Shuku Herman, Chief Medical Officer
From hesitation to confidence in vaccination
Early results show a gradual increase in vaccination coverage in the initial area showing a promising trend toward reducing zero-dose cases. The intervention’s design ensures that fears about AEFIs no longer keep caregivers away from clinics, while home follow-up builds trust and strengthens the relationship between health services and families.
Learning meetings continue to refine the approach, tracking quantitative and qualitative indicators to identify what works, where bottlenecks remain, and how to adapt. From last December through August, 3,752 children received paracetamol to prevent AEFI and 15 children who did experience an AEFI were treated free of charge.
By removing a key barrier to immunization, the AEFI prevention and management intervention is not just addressing a health challenge; it’s creating a blueprint for community-driven, sustainable solutions that can be scaled across the DRC.
The long-term vision, according to Dr. Herman, is clear: "The experience must be shared with the province—why not the whole country?"