Medical oxygen shortages have persisted throughout the COVID-19 pandemic. Although vaccines are rolling out in some countries, many will have to wait years before the majority of their populations are vaccinated. In the meantime, medical oxygen will remain a critical essential medicine.
Most recently, the world’s attention has been on India, where rising infection rates mean demand is outpacing supply—and it has taken a devastating toll. Global efforts to meet immediate needs are ramping up, but building systems for medical oxygen access is complex.
What makes it so complicated? PATH experts Deogratias Agaba and Alex Rothkopf explain what it takes to keep the oxygen flowing.
Weighing the options for oxygen production
Oxygen is an essential medicine and a key treatment for a wide range of conditions, such as obstetric emergencies, premature birth, and pneumonia, that affect all parts of the population. In fact, the need for medical oxygen has been on the rise for more than a decade, as diseases requiring oxygen for treatment are accounting for a larger share of the burden of disease.
Meanwhile, oxygen has been chronically underfunded in low- and middle-income countries for decades.
“The oxygen access gap is not new, but COVID-19 has brought this issue into the light,” says Deogratias Agaba, senior communications officer with PATH in Uganda. “When the pandemic began, many governments tried to prepare, but oxygen systems are difficult to quickly scale. They require significant up-front investments in time and money, and then dedicated resources to maintain.”
Oxygen access involves a slew of sophisticated equipment, along with accessories for measuring and administering the medicine. All of these require training on how to use them as well as regular maintenance.
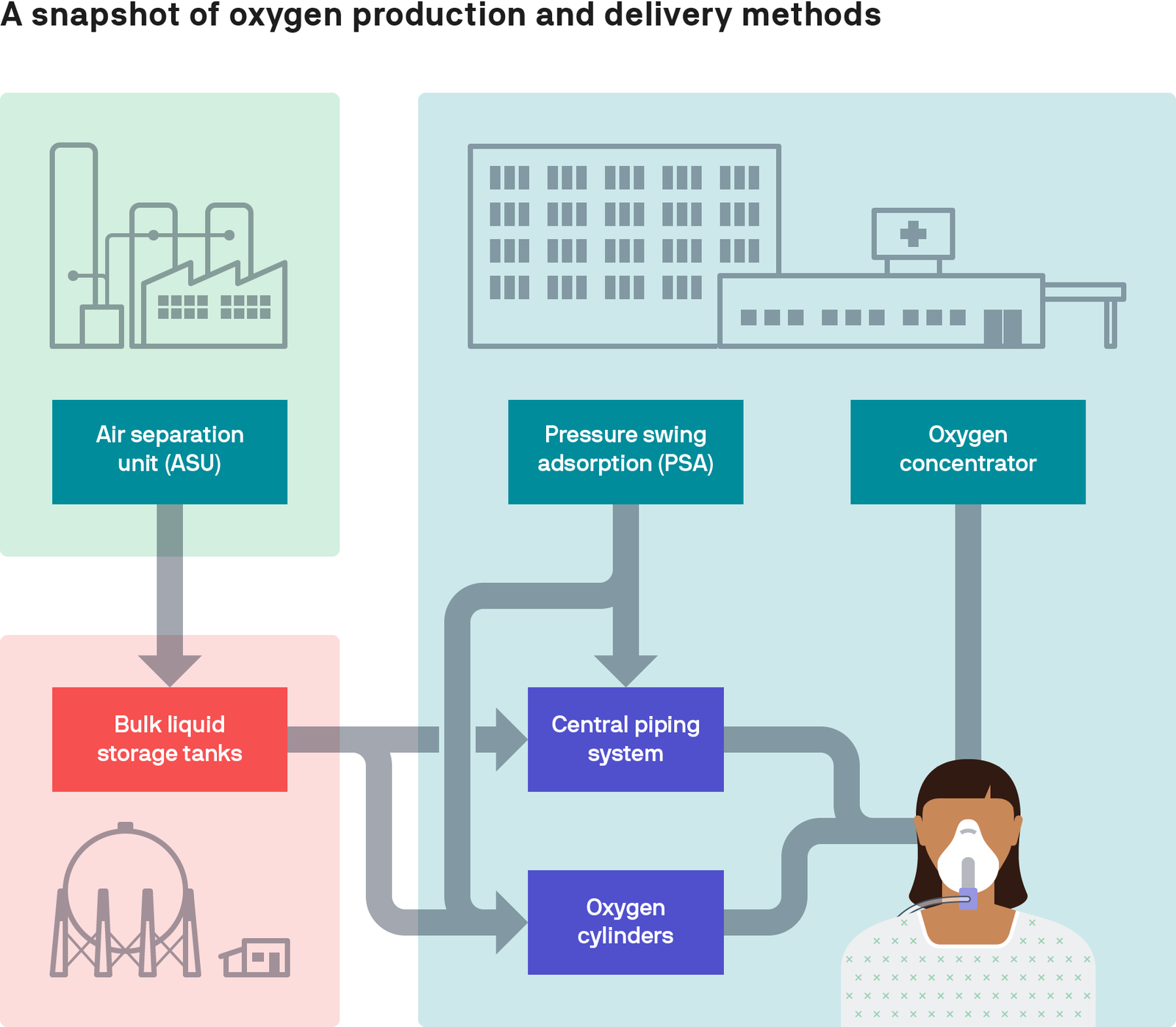
But it all begins with producing or procuring oxygen. There are three main ways oxygen is produced.
Oxygen concentrators draw in ambient air and remove nitrogen, concentrating the oxygen and providing a continuous supply to the patient’s bedside. Concentrators work best in environments with clean air, low humidity, and reliable electricity—and for patients who require lower air flows.
“Because concentrators are a rather simple and comparatively cheap solution, with less infrastructure, logistics, or equipment requirements, they are often the preferred solution during an emergency,” says Alex Rothkopf, supply chain management and data science advisor at PATH.
During the COVID-19 pandemic, aid groups have mobilized to provide these devices to address urgent oxygen shortages—for example, PATH is working with the US Agency for International Development to procure concentrators for India. But concentrators can’t provide the high flows that some COVID-19 patients require. And they aren’t sustainable or scalable oxygen sources.
“Oxygen concentrators are the least effective solution. One unit produces oxygen for one patient. And the products often fall into disrepair due to the cost and complexities of maintaining thousands of units, which often break from surges in electricity,” Alex said. “They shouldn’t be a replacement for long-term solutions.”
But the other options come with challenges as well.
Pressure swing adsorption (PSA) plants are standalone oxygen generation systems that use a flow and compression methodology to extract oxygen from the air. They’re essentially very large oxygen concentrators that can produce oxygen for many patients at once.
These are often the choice for hospitals that generate oxygen on-site. The oxygen can be piped directly to patients’ bedsides, or compressed and stored in gas cylinders and administered from there.
“Building a PSA plant requires complex analysis to ensure its specifications align correctly with the facility’s environmental conditions and, similar to concentrators, they require reliable electricity,” says Alex. “It takes a lot of up-front capital to build, but ongoing operating costs—for technicians, electricity, maintenance, and spare parts—make up a large proportion of total costs. These factors quickly multiply the initial investment.”
Oxygen can also be produced commercially, by large-scale, industrial manufacturers that employ air separation units (ASUs).
ASUs use a process known as cryogenic fractional distillation to produce highly purified liquid oxygen, which is stored in bulk tanks. From there, it can either be converted into gas and stored in cylinders, or poured into a liquid tanker truck to ship to facilities that have a liquid storage tank.
“This is generally how oxygen is produced and delivered to hospitals in most high-income countries, where there is steady demand for medical oxygen and sufficient resources to procure a steady supply,” says Alex. “In larger facilities in low-resource countries, we can expect a similar, stable level of need. But without quantifying that need and building a suitable operational model, it might not be an attractive opportunity for an industrial gas supplier.”
Making the market work for patients
From these three production methods stems a web of subsequent decisions to make around procurement and ownership of equipment, purchasing agreements, delivery, storage, training, and maintenance.
“These systems are incredibly context-specific. PSA plants may work well in a place where electricity is generally reliable and affordable; for example, this is generally the case in Ethiopia. But this won’t be the best option in another place where electricity is expensive,” Alex says.
Similarly, liquid oxygen can be shipped over rather long distances in a cost-effective way, but it requires steady demand and a well-established road network to accommodate a tanker truck with a highly flammable payload.
“There is no one answer—the oxygen production ecosystem in just one country can be incredibly complex,” Alex added. “Most countries will need a mix of different generation and storage solutions to serve the context of each individual hospital and facility.”
How hospitals purchase the oxygen can make all the difference as well. Long-term supply contracts can lower costs and secure steady supplies, but this requires having the financial resources to commit and the available data to forecast long-term needs.
“Conditions vary widely from one health care facility to another. Figuring out how best to procure and implement a sustainable medical oxygen system is technical and complex on its own,” says Deogratias.
Assessing biomedical equipment is a large part of what PATH is doing to support governments with medical oxygen access. This includes rapid assessments of oxygen needs, equipment needs, and a range of factors from climate and location to electricity supply and patient demographics/demand. This information is used to build a road map for increasing access to oxygen.
Once a facility has oxygen, there are additional accessories necessary to administer oxygen therapy to patients: nasal cannula and tubing; accessories to control pressure, flow, and concentration; and pulse oximeters to monitor levels.
Putting the pieces together
Today, low- and middle-income economies need more than 2.4 million cylinders of oxygen (this is changing daily—track current oxygen needs here) to respond to COVID-19. Meeting this record-breaking need will require a systems-level approach to oxygen and its supply chains.
But bottlenecks to oxygen supply chains can happen at many levels: from manufacturing to in-country logistics to shipping supplies.
“To avoid these gaps, we need multisector partnerships. This often means collaborating with unlikely partners,” Deogratias says.
“COVID-19 has been devastating, but it woke people up to the importance of medical oxygen. There is much work left to do, but I feel optimistic.”— Deogratias Agaba, senior communications officer, PATH
For example, the government of Zambia is partnering with the private sector to increase manufacturing capacity, attracting investment for more plants, and financing to ensure hospitals can enter agreements with plants.
“COVID-19 has been devastating, but it woke people up to the importance of medical oxygen,” Deogratias says. “There is much work left to do, but I feel optimistic because there is momentum for sustainable oxygen systems to serve the people who need it.”



