High-quality digital diagnostic devices have the potential to transform health service delivery in primary care facilities. Digital tools can improve health care workers’ speed, quality of care, and engagement with patients, motivating patients to seek diagnoses and continue to engage with the health system.
By replacing paper-based data collection systems with connected diagnostic tools, for example, health care workers could rapidly access and analyze data across multiple diseases—leading to more efficient and effective patient screening and disease management.
Connected diagnostic tools that feed information to national systems could also support the early identification of at-risk patients and comorbidities, shortening lead times to health intervention and treatment plans. Disease data collected through digital diagnostic tools can moreover inform local health strategies, as well as subnational and national disease surveillance efforts.
Lowering barriers to successful adoption and use
However, to be usable and effective, digital technologies must be suited for the environment and system where they will be adopted.
According to the Digital Implementation Investment Guide (DIIG), developed under the framework of the emerging Global Strategy on Digital Health, many new digital health technologies have seen ”limited adoption and success because they were piloted in areas that had inadequate access to electricity and mobile networks or were otherwise inappropriately designed for the context.”
Without reliable electricity, for example, a health care worker cannot use or charge digital devices.
Additionally, health care workers have varying levels of digital literacy. This can make it difficult to use new technologies, accurately interpret data, and develop treatment plans with these tools. This is why introducing new tools must prioritize training in their proper use, interpretation, and management.
It is essential that digital diagnostics strategies consider point-of-care needs and realities, health care workers’ workloads and capabilities, and patients’ confidentiality and trust.
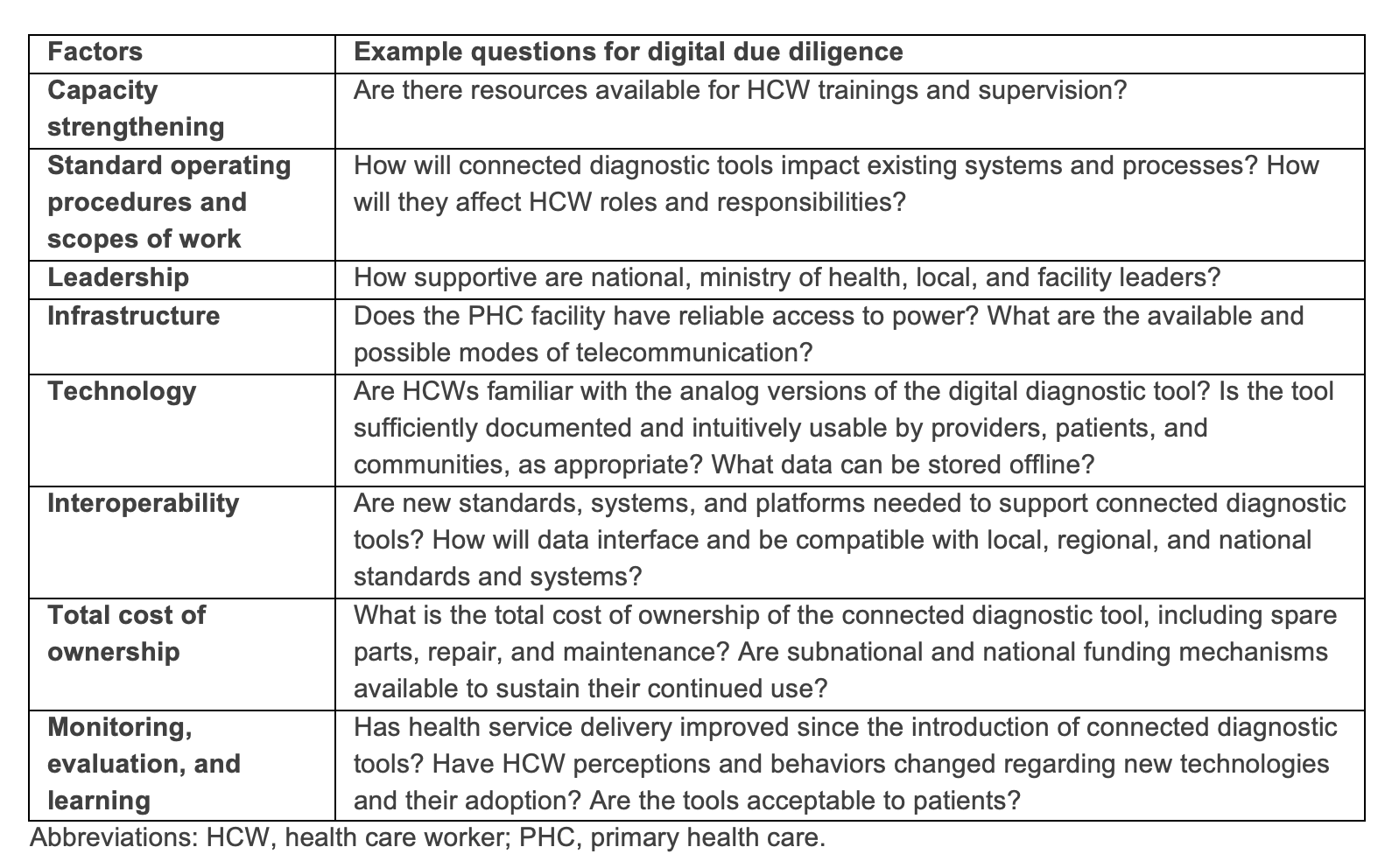
Table 1. Considerations for connected diagnostic tools at the primary health care facility level.
In Kenya, PATH helped introduce digital pulse oximeters at 60 primary health care facilities in three regions. These noninvasive devices measure heart rate and oxygen saturation in the blood and, when used in combination with an electronic clinical decision support algorithm, help health care workers accurately and effectively identify and treat severely ill patients.
The Tools for Integrated Management of Childhood Illness (TIMCI) project, a global effort led by PATH and funded by Unitaid, introduced these tools in Kenya as part of its overall effort to identify severe illness and decrease mortality, particularly in children under five years of age.
PATH selected pulse oximeters for the TIMCI project based on their affordability, portability, and suitability for use with children and neonates at the primary care facility level. PATH and the Swiss Tropical and Public Health Institute developed an accompanying clinical decision support algorithm with a user-friendly interface adapted to health care workers’ needs at the point of care. This included easier access to guidelines from the World Health Organization’s Integrated Management of Childhood Illness strategy.
In this specific situation, the TIMCI project selected pulse oximeters without connectivity features, despite their availability.
“We wanted to make sure that the pulse oximeter could be used in facilities with minimal resources,” said Dickens Omedo Ochuka, Senior Monitoring, Evaluation, and Learning Officer, PATH Kenya. “A connected pulse oximeter would have required functional internet and other infrastructure requirements that are often missing in lower-level facilities.”
In parallel to gathering data and experiences on pulse oximetry, the TIMCI project is also assessing the potential of multimodal pulse oximetry devices that incorporate connectivity features to support a wide range of critical functions in primary care facilities where connected tools are ready to be adopted.
TIMCI project findings offer crucial insights on how health care workers respond to new technology introductions. Dickens believes this could, in part, be linked to whether health care workers see new technologies as the new “shiny toy” or a genuine supportive tool.
”Once health care workers see that outcomes with the tools are better than outcomes without, then they are motivated to use them. Being able to see how device data can be used to identify, treat, and save the lives of severely ill children is motivating,” he says.
Dickens also emphasizes the important role local health managers play in identifying and selecting users who would best benefit from new technologies.
“It’s also important to make mentorship resources available—to accelerate acceptance and adoption of new tools among health care workers,” Dickens says.

A health care worker examining a TB patient at the Chuong My District Health Center in Vietnam. Connected diagnostics can improve patient access to effective and efficient health services in primary care facilities. Photo: PATH/Matthew Dakin.
What is next for connected diagnostics?
Equipping primary health facilities with appropriate diagnostic tools will make the difference between a scalable, sustainable, impactful diagnostics strategy and a fragmented one-off effort that provides limited value to the health system, community, and patients.
The introduction and adoption of connected diagnostic tools in low-resource settings will require a holistic approach where facility capacities, health worker capabilities, national health priorities, digital maturity, and financial resources are thoughtfully considered.
A useful resource could be a tool selection guidebook that features digital and connected diagnostic tools suited for low-resources settings, similar to the Global Goods Guidebook. The development of a such a guidebook would require the joint collaboration of industry partners, academia, and other national, regional, and global stakeholders.
As the field of connected diagnostics continues to grow and evolve, so will challenges that demand the attention of the global health community. PATH is committed to supporting these efforts and will continue to leverage its knowledge and expertise to implement safe and appropriate diagnostic tools and systems where they are needed most.
Explore this article series (linked below) to dive deeper into specific examples of connected diagnostics at national and local levels.



