As the world continues to rapidly digitalize, there are more digital tools available that can improve the quality and use of health data for decision-making.
For example, many countries have started tracking vaccinations with electronic immunization records. However, these systems do little to improve vaccine coverage rates unless the data are used to identify gaps.
Health workers must be able to access past data to identify and communicate with families of children who are behind on their immunization schedules. Similarly, health officials need data to identify areas with low vaccination rates for awareness-raising campaigns.
So how can countries accelerate data use and make the most of digital transformation?
The Data Use Acceleration and Learning (DUAL) project, a partnership between PATH and Cooper/Smith, has focused on answering this question. The DUAL project has learned from the direct experiences of five African countries—Burkina Faso, Ethiopia, Malawi, South Africa, and Tanzania.
The DUAL Model
Through extensive research, interviews with stakeholders from these five countries, and building on previous frameworks, including the National eHealth Strategy Toolkit, DUAL identified and mapped ten elements that are essential for a sustainable digital transformation.
“With these ten elements in place, health workers and health officials will be better able to use data to improve health service delivery,” says Taonga Chilalika, Advocacy and Policy Officer at PATH, who led engagement with the five DUAL focal countries
The DUAL model’s ten elements cover both the technical considerations and the human elements that are foundational to adopting and using digital health and data tools.
On the technical side, for instance, countries may need to upgrade physical infrastructure or existing digital health systems and applications. On the human side, countries may need more digital champions in government or increased technology skills in the health workforce.
These ten elements represent the necessary “ingredients” of successful, holistic digital transformation. They are interconnected and should be addressed together.
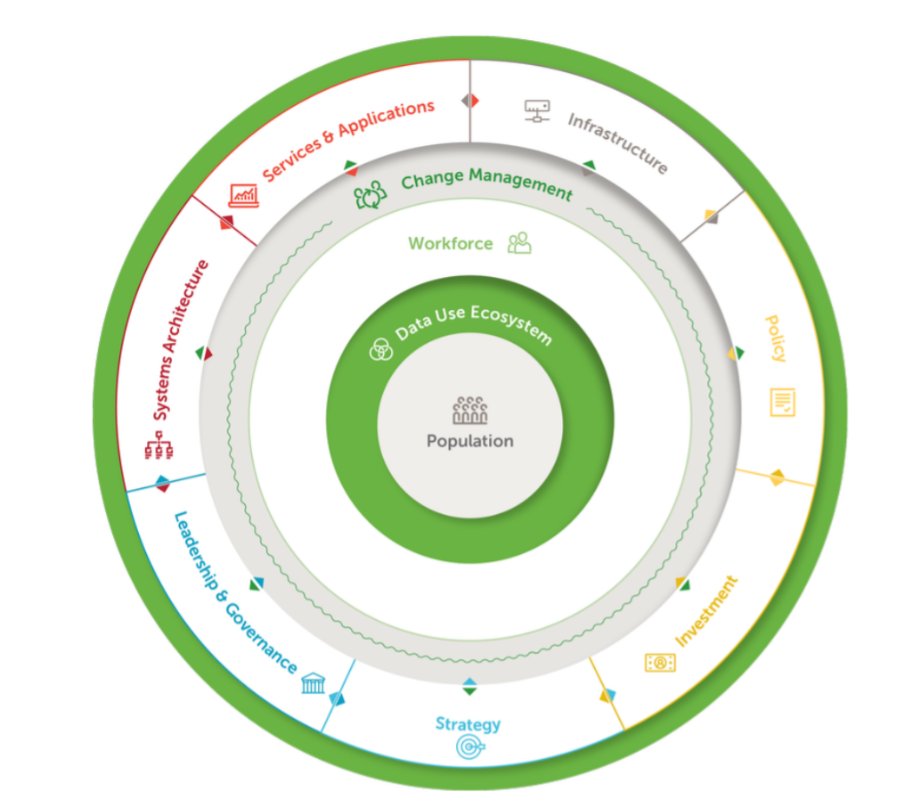
The DUAL model identifies ten critical elements of a comprehensive approach to transforming a country’s health data systems and digital tools to advance data use. Graphic: DUAL.
Putting learning into action
The five countries’ experiences—their successes, challenges, and what they have learned about the enabling factors of digital transformation—present a learning opportunity for the larger global health community.
In addition to the ten elements, the DUAL model suggests specific actions to support each of the ten elements, drawn from successful interventions in the five focal countries.
Countries at any stage of the digital transformation process can assess their health systems against the ten elements to identify areas for intervention. They can then incorporate recommended actions that make sense for their context.
The DUAL model supports a range of digital health stakeholders—country governments; global and regional policymakers; digital health program implementers, including from the private sector and international nongovernmental organizations; and funders operating at a regional or global scale—in collaborating to help digitally transform a country’s health systems in alignment with its health targets.
For example, a key learning for government is to focus resources on building health actors’ technology skills and on activities that motivate and educate health care workers so they feel confident and invested in using new digital systems.
This insight was relevant for stakeholders in Ethiopia.
“To help enhance the data use culture of health workers from different institutions, including health facilities, several capacity-building trainings were administered. Woredas [districts] and especially hospitals where the capacity-building programs have been conducted have shown change with regard to data use culture for decision-making. This was not there prior to the intervention of the project,” says Teklehaymanot Gebrehiwot, Director of the Planning and Policy Directorate at Amhara Regional Health Bureau in Ethiopia.
Based on our findings, the DUAL initiative also identified important recommendations for funders. For instance, it is critical to ensure digital health investments align with a country’s vision, priorities, and strategies. Additionally, funders should align investments with other funders to reduce countries’ and implementing partners’ burdens of coordination.
Pierre Yaméogo, Head of the Universal Health Coverage Technical Directorate in Burkina Faso noted that investment coordination has been important to making progress on digital transformation in his country.
“Donors, other stakeholders, and the private sector have collaborated with us on [digital health] investment priorities through the One Plan, One Budget, One Report project, which started in August 2020. Partners have responded positively to this collaborative process,” Yaméogo says.
Learn more about the DUAL report and recommendations at www.acceleratedatause.org.



