Since well before the 1978 Alma-Ata Declaration, which identified primary health care as key to attaining health for all, significant investments have been made to reduce maternal and child deaths, eradicate polio, and stamp out malaria, tuberculosis, and other infectious diseases. These investments have achieved significant results, including reduced morbidity and mortality from preventable diseases.
However, more could have and can still be achieved if these investments are oriented to have a more comprehensive, people-centered approach that is focused on establishing resilient systems for effective service delivery. These systems must include promotion of healthy behaviors, disease prevention, disease detection, and management of illnesses. This is where primary health care comes in.
Primary health care (PHC) has been proven to be the most cost-effective way to improve population health outcomes. Investing in PHC is not only smart, but necessary if we are to achieve universal health coverage (UHC).
Here are three ways that financing can help strengthen PHC and bring us closer to the global goal of UHC by 2030.
1. Increasing investment in primary health care
Despite ample evidence that primary health care is the most cost-effective way to improve health outcomes, global and national government spending on PHC still falls short. Currently, less than 40 percent of all spending on PHC comes from governments. Average annual government spending on PHC is approximately $3 per capita in low-income countries and approximately $60 per capita in lower-middle-income countries.
These figures are well below what is needed to provide a basic package of essential health services. As a result, almost half the world’s population lacks access to essential health services.
Despite global economic headwinds brought about by the COVID-19 pandemic and the Russia-Ukraine war, new and catalytic investments are still needed to strengthen PHC for effective delivery and better outcomes and to keep pace with our universal health coverage goals. Investments are needed to improve supply chain infrastructure and systems, expand laboratory and diagnostics infrastructure, and reduce the deficit of medical equipment so health care workers can perform basic functions.
Service delivery needs to be redesigned to be provider-friendly and to offer comprehensive and integrated essential services with a people-centered orientation.
At PATH, we are working with country leaders at national and subnational levels to mobilize more resources for PHC. Our work focuses on mobilizing resources for systemic, holistic investments, such as investments in data and digital infrastructure, to optimize delivery systems for improved health outcomes.
2. Efficient, evidence-driven spending
In addition to increasing investments for primary health care, existing and new resources must be efficiently allocated, deployed, and applied to deliver the best possible outcomes for the money spent.
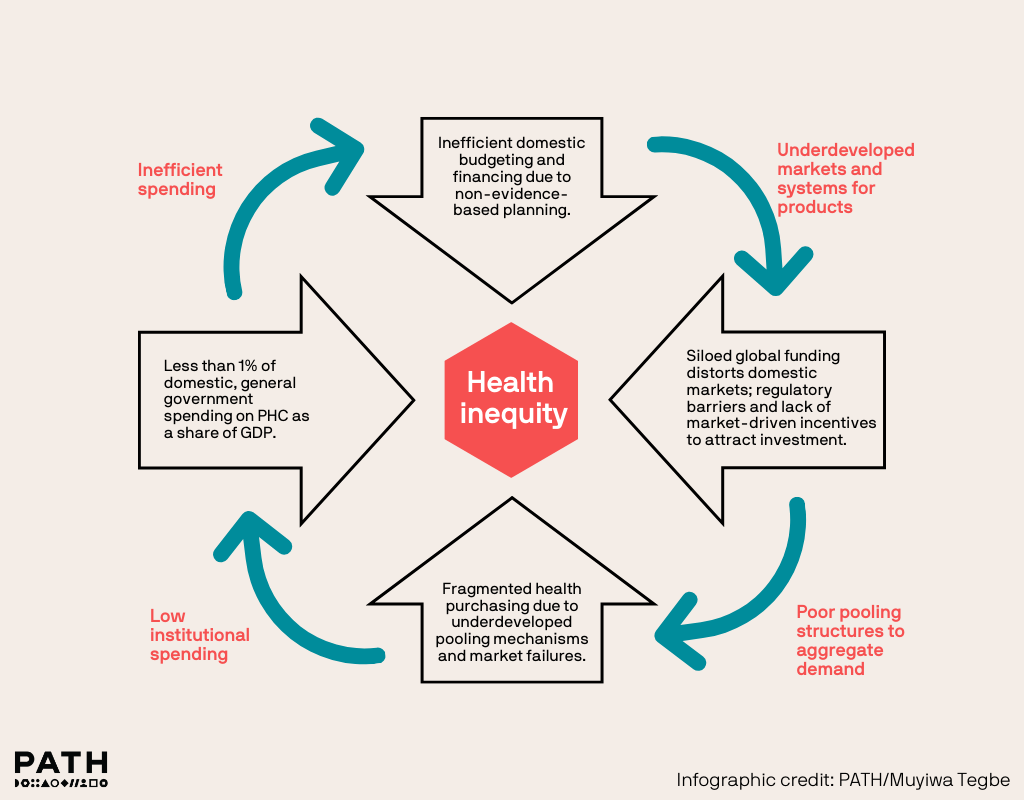
Siloed health funding, limited evidence-based budgeting, and weak markets for health limit capacity for efficient health system spending.
PATH partners with governments to conduct economic assessments to guide the introduction of new services or products. We also work with governments to implement strategies to improve spending efficiency through evidence-based planning and decision-making.
This includes supporting the generation and use of evidence for health sector planning, budgeting, and resource allocation. With better data and information for planning, policymakers can implement targeted resource allocation to address communities’ most pressing needs.
For instance, the Noncommunicable Diseases (NCD) Forecasting Tool for Essential Medicines and Products, developed by the Coalition for Access to NCD Medicines & Products—which includes PATH and others—is a tool that helps policymakers make informed strategic decisions that will lead to more realistic financing and increasingly strategic procurement. Tools and information like this help ensure greater availability of NCD products throughout public health supply chains so that countries can meet the needs of people living with NCDs.
To help communities identify their most pressing needs, PATH is helping design and deploy participatory planning models that will ensure community priorities are understood and reflected in budgets. Finally, as these and other changes are implemented to improve spending efficiency, it’s crucial to monitor spending, understand outcomes, and identify efficiency gains through regular assessments for system efficiency.
3. Resource pooling to improve financial risk protection
Financial risk protection mechanisms are critical for protecting people from catastrophic health expenditures and for increasing access to PHC. However, lack of financial protection pushes more than 100 million individuals and households around the globe into extreme poverty every year.
Risk pooling mechanisms, such as national health insurance schemes or social health insurance schemes, promote equitable access because they eliminate risk of catastrophic direct spending for health and make spending more predictable.
Unfortunately, these mechanisms have not been expanded enough to provide coverage and protection from catastrophic spending for the vast majority of people in low- and middle-income countries (LMICs), leaving households and entire communities at financial risk from unplanned health events.
It is imperative that country governments reexamine their approaches to financial risk protection by exploring the design and implementation of risk protection mechanisms that take into consideration their unique populations.
For instance, LMICs often have large informal sectors with shadow economies and large poor populations that prioritize daily subsistence over saving for health. This makes it difficult for contributory mechanisms to be successful due to the lack of foundational systems to collect premium contributions. Additionally, in many of these countries, confidence in the health system has waned over time.
PATH works with leaders in LMICs to generate insights that inform health systems intervention, including design of risk protection schemes to ensure that they are fit-for-purpose. PATH also supports planning and decision-making at national and subnational levels by conducting economic studies and evaluations that enable understanding of the costs of health programs and/or service delivery and provide evidence on their value proposition.
Such insights have enabled our country partners in Kenya and Uganda to make smart investments to introduce interventions that have enabled delivery of high-quality services that reflect the needs of individuals and their communities.
Financing for our future
After decades of investment in siloed, disease-specific programs and projects, it is time to redirect financial resources toward PHC systems. That is how the global community will achieve UHC. PATH, our partners, governments, and communities must continue working together to build systems that keep people at the center.
When global and national funding is applied to strengthen PHC, it has the potential to expand equitable access to health care and accelerate progress toward universal health coverage.



