




When people are healthy, communities thrive. Give the gift of good health for all.
For millions of people, life-saving services are out of reach. Your gift can change that.
Ways to give
Donors fuel our impact.
Make a difference with PATH. Your involvement powers our work and drives innovation in health. Whether you're contributing as an individual, joining forces through your workplace, or partnering with us on a global scale, your support is the catalyst for change.
A trusted partner
PATH is one of America's Top 100 Charities
PATH is pleased to have been named to Forbes’ annual list of the largest charities in the United States. PATH scored 99 percent in fundraising efficiency and 89 percent in charitable commitment.
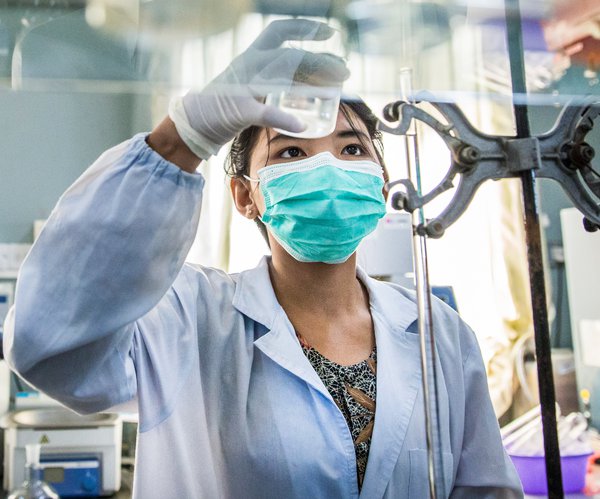
Realizing the vision of universal health coverage
We make good health more accessible for everyone, everywhere.
PATH’s global team of scientists, clinicians, designers, engineers, advocates, and experts from dozens of other specialties all share the same goal: health equity. We partner with public institutions, businesses, grassroots groups, and investors to solve the world’s most pressing health challenges.








